Seamless Credentialing. Get Better Contracted Rates.
We strive to empower healthcare providers by simplifying the medical credentialing and enrollment services, enabling them to focus on their core mission of saving lives.
Elevate Your Practice with Our Expert Credentialing Services—Achieve Seamless Success!
Contact Us Today for a Free Audit and Quote
Crucial Follow-Ups
Our expert medical billing teams ensure that all follow-ups are managed efficiently, streamlining the application process for smooth results.
Continues Monitoring
The insurance payer enrollment process is critical. Our credentialing experts provide ongoing monitoring to ensure successful completion.
Early Risk Identification
Our credentialing experts proactively identify potential risks, acting as a valuable extension of your team to mitigate issues early on.
Provider Enrollment & Medical Credentialing Services
Clinic IT comprehensive medical credentialing services enable healthcare providers to simplify the provider enrollment and credentialing process, avoid claim delays, and save time and resources. With our centralized process and knowledgeable experts, providers can recognize revenue sooner and free themselves from the hassle of handling piles of printed documents and tiring follow-ups.


Benefits of Clinic IT Credentialing Services
With our diligent credentialing and Enrollment services, you get the following benefits:
o Get credentialed faster with all significant payers
o Reduce claim denials and improve cash flow
o Get more patient referrals from the network
o Avoid piles of paperwork with our document management system
o Get support for filling up cumbersome application forms
o Reduce costs of the credentialing process with our global delivery teams
o Get timely reports on the status of your applications
We have helped many providers and practices with the initial credentialing, re‐credentialing, and getting the best out of
their practices.
What Clinic IT Offers
We start with the first step and collect all the required information and documents to file applications. The information and documents are provided by the provider or practice. The documentation requirements vary from payer by payer
New Credentialing
We handle all aspects of credentialing for Medicare, Medicaid, and commercial insurances, covering both individual providers and groups. This includes managing the reassignment of individual providers to groups and ensuring timely credentialing for various insurance types. Our process ensures that credentialing is seamless and compliant, addressing both initial and recredentialing needs.
Provider Data Maintenance – Update Management on Payer Systems
We handle updates to provider demographic information in payer files and maintain accurate provider directories on payer websites. Our services also include managing EFT/ERA enrollments to ensure seamless data integration and accurate payment processing.
Contracts Creation and Maintenance
Our services include drafting and finalizing new contracts for individual and group practitioners. We also update existing contracts to reflect changes such as adding or removing providers and locations, or modifying plan types. Regular reviews and updates ensure that contracts remain accurate and aligned with operational requirements.
Tracking and Analytics
Maintaining a repository of provider’s credentialing documents Maintaining Contracting agreements Tracking credentialing dates, expiration, and alerting dates to initiate credentialing processes Working with the denials team to understand if there are any claim denials due to credentialing issues
CAQH Attestation
We manage the CAQH application process, including quarterly attestations and tracking expirations and renewals. This involves monitoring the expiry dates for essential credentials such as state DEA licenses, board certificates, and malpractice insurance, ensuring all documentation remains current.
Training your staff
Our approach includes discussing audit findings with staff to address risks and implement corrective actions. We provide detailed reports to both physicians and front staff, highlighting strengths and areas for improvement. If specific training needs are identified, we offer targeted expertise to enhance staff performance and compliance.
Develop Effective
Audit Strategy
Our auditors will decide on a prospective or retrospective strategy after reviewing medical claims to ensure the most effective approach.
Examine Records
In EHR
We meticulously review billing reports, charges, and codes in the EHR to enhance cash flow and reduce claim denials.
Rectifying
audit Contest
We address any issues found in our detailed report quickly. Clients can challenge audit findings within 60 days if there are disagreements.
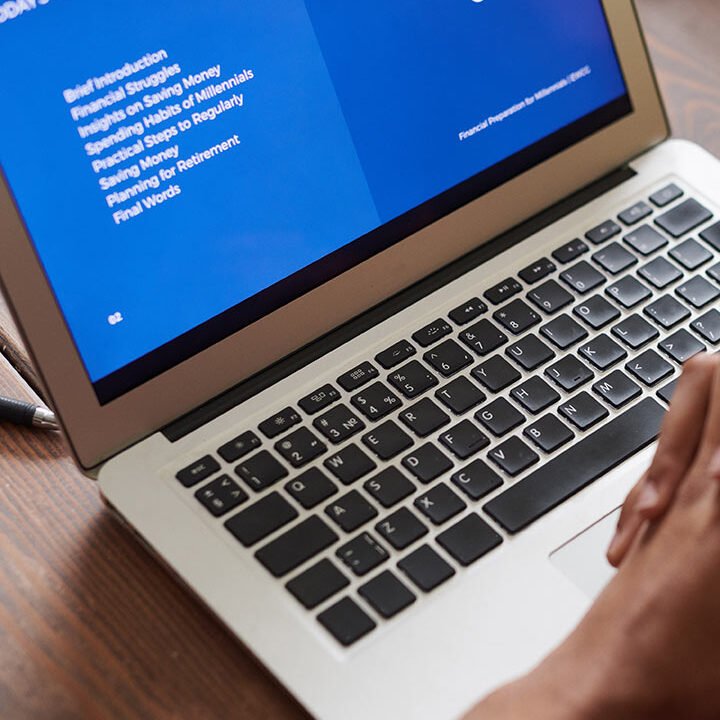
Medical billing and the code compliance audit process
Our Clinic IT CRM department provides free consultations to outline how our internal auditing process will be performed on your prepared medical claims.
Your Expert Partner in 50+
Medical Specialties
- Internal Medicine
- Family Medicine
- OB/GYN
- Cardiology
- Gastroenterology
- Pediatrics
- Podiatry
- Psychology
- Mental Health
- Dermatologist
- Urgent care
- Neurology
- Nephrology
- Endocrinology
- General surgery
- Physical medicine
- Pulmonary
- Radiology
- Orthopedic
- Obstetrics


Testimonials
Dr. Giancarlo / French Medical Health
Dr. Usman Khalid / Pride Health Wellness
Dr. Yvonne, Health Clinic
Frequently Asked Questions from Our Community
We cut through today’s complexity and use whatever technology it takes to get you where want to be.
What does your credentialing services include?
Our credentialing service includes verification of licenses, certifications, and training; background checks; credentialing with insurance companies and networks; and ongoing monitoring and re-credentialing.
How long does the credentialing process take?
The credentialing process typically takes 60 to 120 days, depending on the complexity and the responsiveness of the providers and verifying agencies. We strive to expedite the process as much as possible.
How often does credentialing need to be renewed?
Credentialing must be renewed periodically, usually every 2 to 3 years, depending on the requirements of the accrediting bodies and insurance companies.
What are the common challenges in the credentialing process?
Common challenges include delays in verification of credentials, incomplete documentation, and discrepancies in information. We help manage and resolve these issues to ensure a smooth process.
Who is responsible for the credentialing process?
The responsibility typically falls on healthcare providers and their administrative staff. However, outsourcing to a credentialing service can streamline the process and reduce the administrative burden.
How can I check the status of my credentialing application?
You can check the status of your application by contacting our office directly. We provide regular updates and are available to answer any questions you may have throughout the process.




















Ready to Get Started?
Contact Us Today for a Free Audit and Quote
- Transparent Reporting
- HIPPA Complined Traniend Staff
- Dedicated Appeal Department
- Dedicated QA Department